As 2024 draws to a close, the Center for Connected Health Policy (CCHP) is releasing its annual roundup of state telehealth legislation. This year, state legislatures continued to refine, expand, and impose new standards on telehealth, responding to evolving needs in healthcare delivery and leveraging lessons learned from the COVID-19 pandemic. Notably, increasingly specific requirements for various telehealth modalities, including remote patient monitoring and audio-only services, demonstrate states’ efforts to ensure telehealth remains accessible and aligns with high standards of care.
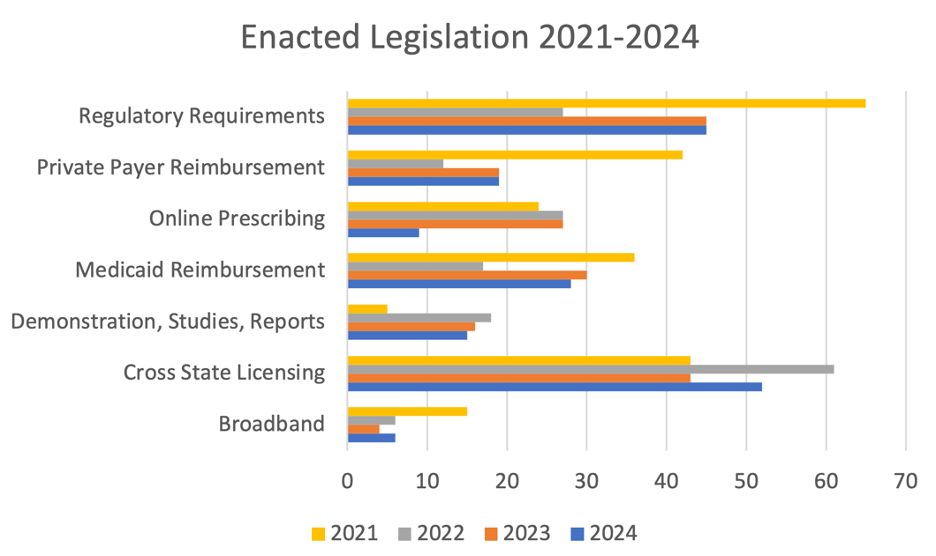
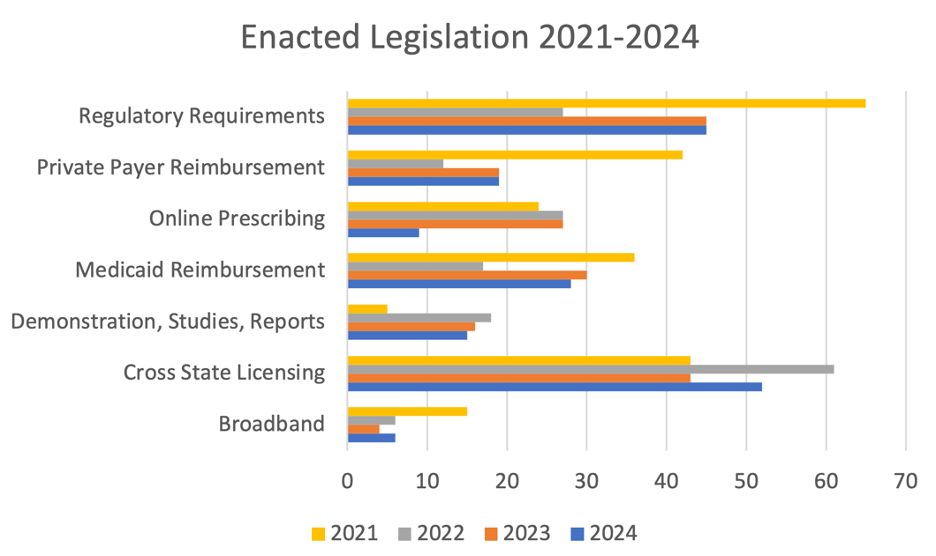
In the 2024 session, CCHP found that 41 states and the District of Columbia introduced telehealth-related legislation. In total, there were 176 enacted legislative bills in the 2024 session, slightly up from the 171 legislative bills last year (2023), marking continued, yet measured, interest in telehealth policy. Bills addressing cross-state licensing had the most significant increase among those passed. Every other category tracked by CCHP remained mostly steady compared to the previous year, including legislation targeting telehealth for Medicaid and private payers. As states confront issues like digital equity, licensure flexibility, and healthcare access, telehealth remains a critical focus of state legislative efforts, showcasing its growing role in the healthcare landscape.
CCHP’s 2024 roundup of approved state legislation, complete with detailed bill summaries by topic area and state, is now available. Below, you’ll find in-depth summaries for each key area in telehealth legislation this year.
MEDICAID REIMBURSEMENT
In 2024, CCHP tracked 28 state bills related to Medicaid reimbursement that were enacted, marking a slight decrease from 2023, when 30 such bills were passed. States continued to expand Medicaid coverage for a variety of healthcare services offered via telehealth, including new categories of healthcare providers and services eligible for reimbursement. Kentucky’s SB 111, for example, included speech therapy as a covered service, making it available for in-person or telehealth delivery under Medicaid. By adding these services, states are working to fill gaps in care through telehealth and increase access for Medicaid recipients. Some states took additional steps to broaden the scope of Medicaid-covered telehealth services to specific populations. Colorado’s HB 24-1045, for instance, added substance use disorder (SUD) treatment to the definition of a health-care or mental health-care service in the state’s Medicaid telemedicine statute, effectively requiring the services to be reimbursed at the same rate as in-person care. It also stipulates that Medicaid may provide reimbursement to a behavioral health facility that serves as the originating site at the time of the service. This focus on mental health and substance use disorder treatment reflects a wider trend among states to expand access to behavioral health care through telehealth.

Certain states have underscored the importance of supporting Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs) by enabling them to serve as both originating and distant sites for telehealth. Mississippi’s HB 970 reinforced this approach by ensuring that FQHCs, RHCs, and Community Mental Health Centers (CMHCs) are eligible for Medicaid reimbursement when providing telehealth services at both ends of the interaction. Michigan’s HB 4213, likewise, specifies that a telemedicine service is an allowable encounter for an FQHC, RHC, or tribal health center in the medical assistance program.
Several states have taken strides to ensure Medicaid payment parity, requiring reimbursement for telehealth services at levels comparable (or the same) to in-person services. In the 2024 session, Michigan SB 747 mandated payment parity within the state’s Medicaid program, guaranteeing that behavioral and physical health services delivered via telehealth would be reimbursed at the same rate as face-to-face encounters.
In previous years, audio-only services saw significant expansion across Medicaid programs, but with most programs now reimbursing this modality, the focus has shifted. In 2024, legislation more frequently addressed reimbursement for remote patient monitoring (RPM), highlighting the growing emphasis on supporting advanced telehealth technologies. For example, Louisiana Medicaid is now required by HB 896 to cover a one-time installation and training reimbursement for RPM services, as well as coverage for assessment and monitoring of clinical data for patients that meet certain criteria. Some Medicaid programs also focused in on diabetes, and continuous glucose monitoring. Colorado’s SB 24-168, for example, established a grant program to support remote monitoring in rural and underserved areas, while also requiring Medicaid coverage for continuous glucose monitors. Other states, addressed reimbursement of remote ultrasounds and non-stress tests used in maternal care. For instance, in Maryland, HB 1078 mandated Medicaid coverage for remote fetal non-stress tests and ultrasound procedures. These additions indicate an ongoing trend of states leveraging telehealth technology to improve healthcare access for individuals with chronic or complex medical needs, ensuring that telehealth can meet the diverse and evolving demands of Medicaid populations.
PRIVATE PAYER REIMBURSEMENT
This year, CCHP tracked 19 state bills addressing telehealth private payer reimbursement that were enacted, equalling 2023 when 19 such bills were passed. Pennsylvania passed a private payer law for the first time, SB 739, which mandates that health insurance policies must cover telehealth services provided by a network provider, and may not deny coverage solely because the service took place by telemedicine. Payment cannot be conditioned on the use of a specific proprietary telemedicine technology or vendor.
In 2024, a few states also enacted legislation to ensure telehealth parity, requiring private insurers to cover and reimburse telehealth services comparable to in-person care. Michigan’s HB 4579 mandated coverage parity and established that health plans cannot restrict telehealth services to be delivered exclusively through third-party entities, thereby preserving provider autonomy and expanding patient choice. Seeking to provide continuity with COVID-19 pandemic policies and avoid a sudden change in telehealth reimbursement, Connecticut’s HB 5198 made some pandemic-era telehealth policies permanent, including private payer payment parity, and New York’s S 8307extended telehealth reimbursement parity requirements until April 2026.
PROFESSIONAL PRACTICE REQUIREMENTS
This year, 45 enacted bills dealt with professional requirements around telehealth (which remained steady with 2023, which also had 45 enacted bills dealing with professional requirements). Often, laws explicitly state that specific types of healthcare professionals are permitted to deliver services via telehealth to eliminate any ambiguity that could arise from the absence of clear guidance. Alaska’s HB 126, for example, authorized associate counselors to provide services via telehealth, as long as they are located at an eligible clinic, facility, or private office and the provider is acting within their scope of responsibilities. Illinois addressed additional areas, such as physical therapy with HB 5087. Kentucky’s SB 255 introduced social work telehealth standards, detailing practice requirements to uphold professional integrity across telehealth services, and New Hampshire’s SB 403 authorized certified community health workers to provide telemedicine services. By establishing these standards, states are ensuring that telehealth remains a reliable and high-quality option for patients across diverse fields.
In the veterinary field, telehealth standards were reinforced and expanded. Colorado’s HB 24-1048 permitted telehealth for veterinary services, while mandating an in-person examination to establish a veterinarian-client-patient relationship, subsequently allowing other veterinarians at the same physical premises to participate in telehealth services under the established relationship. Similarly, Florida’s HB 849 addressed veterinary telehealth, outlining appropriate practice requirements. These measures reflect a shift towards telehealth in veterinary care, ensuring that telehealth is integrated responsibly while maintaining quality of care.
PRESCRIBING
Nine enacted pieces of legislation specifically focused on online prescribing requirements in the 2024 legislative session. Often, these prescribing requirements were integrated into broader telehealth professional standards, resulting in overlap; 3 bills addressed both online prescribing and professional standards simultaneously. An example is Tennessee’s SB 2136, which established guidelines for physicians collaborating with physician assistants in a remote healthcare setting, and within the guidelines specifically addressing prescribing protocols.
Additionally, Delaware’s SB 331 addressed out-of-state practitioners prescribing controlled substances, requiring these providers to obtain a Delaware-controlled substance registration and hold appropriate state licensure. The bill specifies that licensure can be obtained through various options, including an interstate compact or interstate telehealth registration.
LICENSING
In total, CCHP tracked 52 enacted cross-state licensing bills, up from 43 enacted bills from the previous year. Several states implemented exceptions to traditional licensing requirements to enhance telehealth accessibility and accommodate out-of-state providers under specific conditions. Alaska’s SB 91, for example, addressed an exception from licensing requirements for out-of-state providers participating as part of a multi-disciplinary team within the state under certain circumstances. California also made targeted exceptions to support specific patient populations. SB 233, for instance, permitted Arizona-based physicians to provide abortion-related care to Arizona residents traveling to California through November 30, 2024, provided they register with the appropriate California medical board. However, this narrowly defined exception has already expired. Likewise South Carolina’s H 4159 creates licensing exceptions for out-of-state practitioners, including in cases of an informal consultation or second opinion, provided that the authority and responsibility for the patient’s care remains with the physician licensed in-state, and where an in-person physician-patient relationship is established in another state for specialty care and treatment is ongoing by that out-of-state provider. See the bill for additional details.
A few states also introduced telehealth-specific registrations to streamline the licensing process for out-of-state providers. Colorado’s SB 24-141 authorized healthcare providers licensed in other states to deliver telehealth services to Colorado patients upon registering with the relevant regulatory body. This approach enables Colorado to maintain oversight while increasing healthcare access for residents, particularly in areas where there may be shortages of in-state providers. In addition to licensing exceptions and telehealth-specific registrations, some states are eliminating outdated licensure requirements that could hinder telehealth’s growth. Indiana’s SB 132, for instance, removed the necessity for out-of-state telehealth providers licensed in Indiana to file a waiver of jurisdiction certification.
Interstate licensure compacts continue to be the most popular way to address cross-state licensing issues. CCHP tracked several bills that joined states to the Audiology and Speech Language Pathology Compact, Interjurisdictional Psychology Compact (PSYPACT), Interstate Medical Licensure Compact, Nurse Licensure Compact, Physician Assistant Compact, Professional Counseling Compact, Occupational Therapy Compact, and Social Work Compact, during this legislative session, with the Social Work Compact and Counseling Compact having the largest jump in states joining the respective Compacts this year. Additionally, a new compact, the Dietitian Compact, debuted this year, with three states enacting legislation to implement it.
PILOTS & STUDIES
CCHP tracked 15 bills that included a telehealth study, pilot or demonstration project that were enacted (down from 16 in 2023). When examining pilot program legislation, a few key themes emerge. The first is a focus on maternal and women’s health. Maryland’s enacted bills, SB 950 and HB 1127 are an example. The bills authorize reimbursement for sexual assault forensic exams conducted via telehealth and also require the Maryland Sexual Assault Evidence Kit Policy and Funding Committee to study the feasibility of using telehealth for conducting forensic exams. These telehealth-based programs demonstrate a commitment to addressing the unique healthcare needs of mothers and vulnerable patients, while enhancing the quality and reach of healthcare delivery.
States are increasingly exploring ways to integrate telehealth into the criminal justice system to improve healthcare access for individuals involved with courts and corrections. This is evident in Oregon’s HB 4002 which targets opioid use disorder treatment in jails, allowing the use of telehealth for addiction treatment and transition planning services.
Artificial Intelligence (AI) related legislation specifically tied to telehealth saw limited movement at the state level in 2024, with the only enacted legislation coming in the form of pilot programs and studies in Maryland. Note that CCHP only tracks AI legislation that directly references telehealth or remote care in some way. In 2024, Maryland introduced AI pilots including HB 582 and SB 473 which launched the Baltimore Innovation Initiative Pilot Program, incentivizing technology startups that propose projects incorporating AI or machine learning in healthcare. Additionally, Maryland’s SB 818 mandates data inventories on AI systems used in healthcare, followed by recommendations for broader applications of AI in healthcare delivery. These initiatives signal Maryland’s commitment to exploring AI’s potential to enhance healthcare efficiency and outcomes, setting the stage for increased AI integration in clinical settings.
BROADBAND
During the 2024 legislative session, CCHP tracked 3 successful broadband-related bills, a slight decrease from 2023, which saw 4 bills enacted in three states. It is important to note that these were not all broadband bills generally, but more specifically those that explicitly mentioned telehealth or remote care. Examples include Colorado’s HB 24-1336 authorizes the office to conduct studies to assess broadband, establishes a work group of stakeholders and creates grants for middle mile infrastructure. Oregon’s HB 4040 creates the Oregon Broadband Advisory Council, which must include one member that represents telehealth.
CONCLUSION
In 2024, state legislatures demonstrated a concerted effort to further refine telehealth policies, with an emphasis on expanding access while implementing standards across various modalities and specialties. Cross-state licensing and telehealth registration processes also remained a focus as states sought to streamline regulatory barriers while maintaining oversight, evidenced by new laws in states such as Virginia and Colorado. As federal Medicare COVID-19 flexibilities near their potential expiration at the end of 2024, states are actively advancing more expansive telehealth reimbursement policies. These efforts include expanding telehealth coverage in Medicaid programs and, in some cases, implementing mandates for private payer reimbursement—avoiding the restrictions on patient location and provider type found in permanent Medicare reimbursement policy.
The developments of 2024 illustrate a broader push toward sustaining and strengthening telehealth’s role in healthcare delivery. As states continue to balance regulatory oversight with the flexibility required for effective telehealth implementation, telehealth is increasingly recognized as a permanent fixture within the healthcare landscape. As we look ahead, the ongoing evolution of state and federal policies will be pivotal in defining telehealth’s future, enabling it to deliver care that is accessible, equitable, and aligned with the highest standards.
For more insights on the federal landscape and what to anticipate in 2025, stay tuned for upcoming newsletters from CCHP. For more on the enacted legislation CCHP traced in 2024, see our 2024 Legislative Roundup Report. |